When Doris, a 30-year-old civil servant suffered series of successive pregnancy failures, she and her spouse were encouraged to seek specialized pregnancy care service.
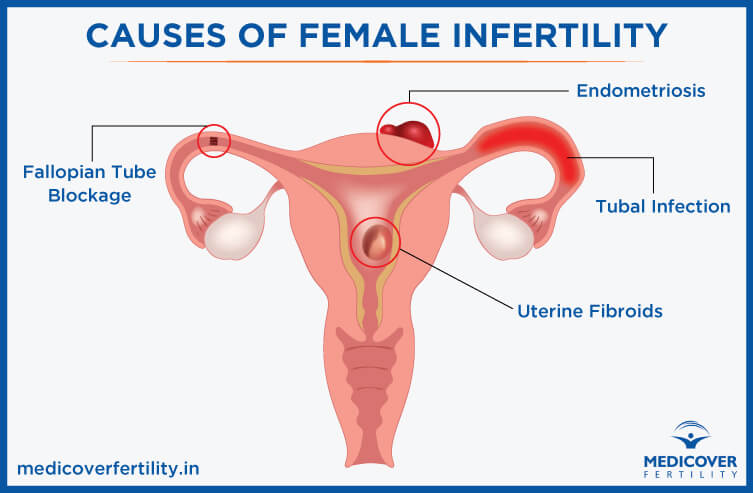
Before then, the couple had tried to conceive for more than six years going from one doctor to another until a gynaecologist diagnosed Doris with incompetent (blocked) fallopian tubes and referred her to a fertility specialist.
After series of preliminary tests and investigations, the couple was advised to try Invitro Fertilisation, IVF, but was in for a shock to learn that it would cost between N1 million and N1.5 million for a single cycle of the procedure. This sum, it was gathered, excludes the cost of assessment, tests, drugs and other incidentals.
The couple’s anxiety escalated when it was made clear that for best results, patients undergoing IVF treatment are recommended to budget for a three-IVF cycle plan.
In Nigeria an estimated 90-95 per cent of IVF and other treatment costs are paid out-of-pocket with just a handful of patients having access to some form of financial support plan. Doris and her spouse belong to the out-of-pocket paying group.
The foregoing exemplifies the financial challenge of seeking assisted fertility treatment in Nigeria where raising children is already challenging under the prevailing economic downturn.
Though most infertile couples readily seek at least one type of fertility treatment, high cost is a major hindrance to achieving their dream of parenthood.
Reproductive health officials told Vanguard that for couples that require donor eggs, donor sperms, or donor embryos plus any additional form of third party intervention such as surrogacy or other technically specialized procedure, the cost is often several times more than that of a normal IVF cycle because there are additional charges to contend with.
Vanguard gathered that infertility treatment costs are not fixed across board, rather costs are usually personalised.
It was further learnt that major factors that determine the cost include the patients’ diagnosis, recommended procedure, as well as the location and sophistication of the treatment centre.
Most of the centres are based in Lagos in Ikeja, Surulere, Ikoyi, Victoria Island and the Lekki/Ajah axis. Several other centres are in the Federal Capital Territory, FCT, Abuja, Port Harcourt, and Asaba to mention a few.
Vanguard findings show that the cost of a routine diagnostic test for infertility ranges between N150,000 and N300,000. This may include semen analysis, blood tests for hormone levels, biopsy, genetic testing, etc.
A medical consultation along with an initial assessment may be offered at a one-time cost of around N100,000. A reassessment is often necessary after six months of the initial assessment at additional cost.
One of the ART consultants told Vanguard that the cost of a standard Intrauterine Insemination, IUI, cycle (including cost of drugs), ranges between N300,000 and N500,000 while subsequent/repeated IUI cycle goes for N250,000 and up to N450,000.
He explained that one of the key determinants of the cost is the location of the centre where the procedure is carried out.
Vanguard findings reveal that in Nigeria, the cost of a single IVF cycle in a decent centre or hospital begins from around N1.0 million up to N1.5 million excluding the cost of drugs. For a two-cycle plan, the cost is between N1.6 million and N2.6 million while a three-cycle plan is in the range of N2.1 million up to N3.6 million all excluding the cost of drugs.
If the cost of drugs is factored in, the overall cost could go up by at least an additional N1 million for each category.
Additional costs for other interventions
It was further disclosed by the practitioners that couples that require additional intervention pay extra.
For instance, the cost of opting for one cycle of a combination of IVF plus Intracytoplasmic Sperm Injection, ICSI, (a technically sophisticated procedure for addressing sperm related male-factor infertility) is between N2.0 million and N3.0 million.
Each subsequent cycle of IVF with ICSI combination is between N1.5 million and N2.5 million depending on the treatment centre.
For couples that require donor eggs, cost of a single IVF cycle is between N2.4 million and N3.1 million inclusive of screening of the donor but excluding the cost of drugs.
For two IVF cycles with donor eggs, couples pay from N4.8 million up to N6.0 million, while the cost of a three-cycle IVF plan with donor eggs goes between N5.5 million and N6.7 million inclusive of screening of the donor but excluding the cost of drugs.
Subsequent repeated cycles with donor eggs start from around N2.4 million per cycle with the cost of drugs adding at least N1 million extra to each category.
Vanguard learnt that if donor sperm is required for the IVF cycle, the costs vary, as sperm banks and fertility centres fix their own prices. The procedure per cycle is between N1.3 million and N1.8 million inclusive of insemination and screening of the donor but excludes the cost of drugs.
One frozen embryo transfer (FET) cycle including the cost of drugs ranges between N0.9 million and N1. 6 million depending on the centre and its location.
For couples that desire to preserve their embryos, the cost of embryo freezing per quarter (per embryo) at average of N100,000.
Other service charges
Endoscopy is an investigative /diagnostic procedure where a thin, lighted tube (endoscope) is inserted into the uterus to examine it for infections, diseases or any abnormalities.
The most frequently carried out gynecological endoscopy procedures are hysteroscopy and laparoscopy.
The cost of these procedures range from N300, 000 up to N3.0 million depending on the patient’s diagnosis/requirements and location of the fertility clinic or centre.
From findings, average cost of basic fertility treatment in Nigeria including consultation, investigation, counselling tests, drugs and follow up starts from a conservative N1.3 million.
Cost of surrogacy higher
If for any reason, a woman is unable to carry her own pregnancy, a surrogate can do it for her. Surrogacy is the involvement of a third party in the infertility treatment process. There are two types of surrogacy – traditional and gestational.
Traditional surrogacy uses the biological father’s sperm to artificially inseminate the surrogate mother who then carries the baby for the intended parents.
A traditional surrogate shares a genetic connection with the baby she carries.
For gestational surrogacy, IVF is utilised to create an embryo that is then carried by the surrogate, thus the surrogate has no genetic ties with the baby since her eggs are not used. This is the more commonly utilised method.
The average cost of gestational surrogacy varies and could range between N5.0 million and N8.0 million or more depending on whether or not it includes the IVF treatment fees, surrogate fee, diagnostic assessments, drugs, legal fees among other costs.
Overseas option still higher
Further investigation reveals that infertility treatment is even more expensive abroad. In the United Kingdom for instance, similar treatment procedures would attract around N3.0 million excluding the cost of visas, flight tickets, accommodation, feeding and other ancillary charges.
In the United Arab Emirates which has become the hub of medical tourism lately, the same treatment would attract up to N3.3 million; USA N5.5 million; South Africa N2.1 million; India N1.8 million; Germany N2.7 million; Spain N2.8 million; Denmark N2.6 million; Greece N2.3 million and Czech Republic N2.2 million
Practitioners explain the cost
Professor Osato Giwa –Osagie, renowned IVF specialist and Co-pioneer of IVF in Nigeria, says the high cost of IVF treatment in Nigeria is not unconnected with the poor state of the economy as well as infrastructural and manpower challenges in the health sector.
Giwa-Osagie encouraged the setting up of even more fertility centres as well as intensive financial support.
“Most of the things utilised in IVF are imported and some are consumables that are used just once and discarded.
“Getting appropriately trained and qualified personnel like the nurses, embryologists and clinicians is still a challenge.
“The equipment is expensive and most centres have to acquire more than one, sometimes two or even three equipment of the same kind for just one procedure because of the issue of maintenance locally. All this adds to the cost.”
According to the “Biological and Social Aspects of Human Infertility: A Global Perspective” published in the Oxford Research Encyclopedia: “Progress for lower-cost state-of-the-art infertility treatment options is desirable.
“However, progress will depend on getting policies right, building health systems that work well and ensuring availability of enough trained medical staff.”
Nigeria’s health funding
For Nigeria, this would include an increase in per capita expenditure within the health system to meet WHO recommendation.
Nigeria has been far behind the recommendations and also behind peer group of nations in healthcare funding, a situation that has forced almost all infertility treatment to be on out-of-pocket expense.
In 2018, as stated by the latest available data by the World Bank, the per capita health expenditure for Nigeria was $84.
In comparison, figures for other developing countries are: Algeria $256, Brasil $848, Gabon $218, Ghana $78, India $73, Kenya $88, Mexico $520, Namibia $471, Pakistan $42, Rwanda $58, Senegal $59, South Africa $526, Tunisia $252, and Uganda $43.
Nigeria has never met the Abuja Declaration target of allocating at least 15 percent of the overall national budget to health.
The closest that the country has got to the target was in 2012 when N289, 770 billion or 6.23 percent of the N4, 648,849 billion federal budget was allocated.
In 2001 when the Abuja Declaration was made, the federal health budget was N41, 269 billion which was 4.46 percent of the N894, 214 billion overall federal budget.
The lowest percentage allocation to health since the Declaration was in 2010 when N185, 765 billion (4.20 percent) of the N4, 427,184 billion federal budget was allocated.
In 2021, the federal allocation to health is N604,191 billion, or 4.45 percent of the N13, 588, 027 billion federal 2021 budget.
This is lower than in 2020 when N575, 228 billion or 5.32 percent of the N10, 810.800 billion federal budget was allocated.
Vanguard News Nigeria
Related